Orthopedic medicine has come a long way over the years, with some of the most important steps being taken in recent history. Advancements in the field have enabled many people around the world to lead more active and healthier lifestyles. These advances have also served to improve the quality of life for those living with debilitating orthopedic conditions such as arthritis, scoliosis, or spinal injuries. With techno-savvy advancements, however, there is no limit to what orthopedic medicine can do in the future.Below is a list of some of the most remarkable advances in orthopedic medicine;
1. X-rays
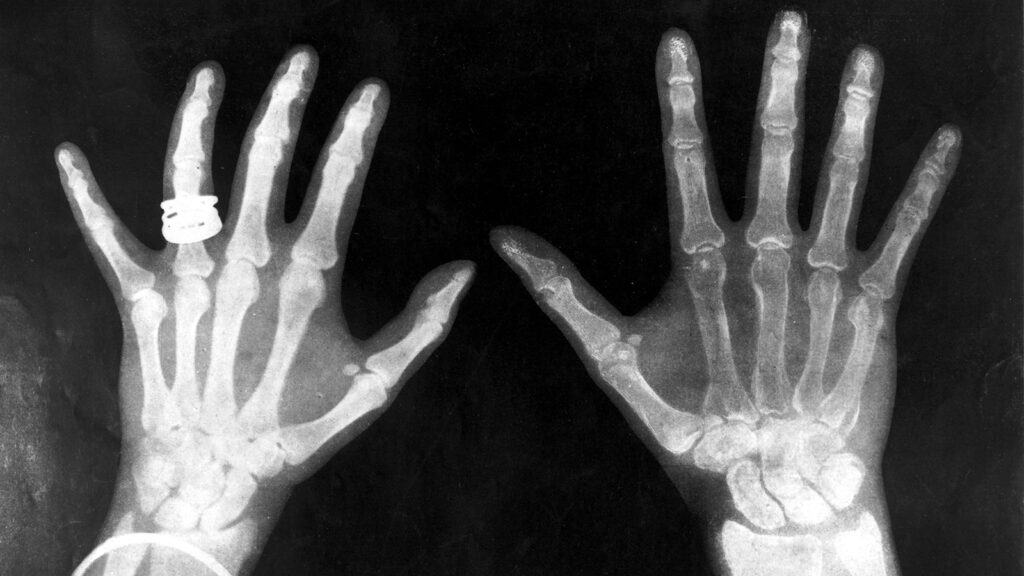
Over the years, X-rays have become more and more effective. Beginning in the 1960s, the use of X-rays became widespread due to the development of new technologies and techniques. As decades went on, advances were made in X-ray equipment as well as image interpretation, which led to a higher degree of accuracy.
These advancements have allowed physicians to get a better look at muscles, tendons, and joints with greater ease. Orthopedic surgeons can now provide more precise treatment with less invasive procedures, as well as better surgical outcomes and shorter healing times.
It is important to note, however, that X-rays are not recommended for everyone. Specific groups of people should be wary of having an X-ray taken. These include the very young, very old, pregnant women, and people with immune system deficiencies or allergies to metallic objects. For these people, CT scans or MRIs may be more suitable forms of imaging technology.
2. Bone cement
Applicable in arthroplasty, kyphoplasty, and vertebroplasty surgeries, bone cement has become an important tool in orthopedic medicine. It is used to treat fractures and regenerate bones by filling defective areas. There are several types of bone cement such as cortical, cancellous, polymethylmethacrylate (PMMA), and poly-L-lactic acid (PLLA) with the polymerization time variable depending on the type.
According to a recent study, PMMA bone cement remains the most commonly used in orthopedic surgeries, with the site of application ranging from ankles, knees, and shoulders to vertebral columns. The same study showed that cortical bone cement was used in spinal fusions and vertebroplasty procedures, as well as in arthrodesis/arthroplasty surgeries. The use of PLLA cement has been shown to reduce the rate of postoperative complications significantly by reducing bleeding and inflammation.
3. Intramedullary nailing technology
In the last decade, Intramedullary nailing technology has come into its own, with a steady rise in demand for the procedure. This technology involves placing a long rod or nail inside the bone of a fractured or broken limb so that it can heal faster and in a better position. The device supports the weight of the body and helps to prevent any further damage to broken bones. Nailing can be used in most kinds of orthopedic treatments (both surgical and nonsurgical).
Long bones (such as the radius, femur, and tibia) can be nailed in single or multiple locations to provide support. Alternatively, it can be used to stabilize joints (notably on the elbow and knee). Intramedullary nailing is also valuable in situations where fusion is not an option due to bone loss or poor bone quality.
4. Engineered Stem Cells For Bone Regeneration
Engineered stem cells for bone regeneration are considered a fairly breakthrough in orthopedic medicine. A technique that involves taking stem cells from a patient’s body fat, the procedure allows the doctor to manipulate these stem cells so that they will be able to grow new bone and repair injured or damaged bone.
Because this procedure utilizes the patient’s own body, it is less expensive than getting artificial bone-implant materials from donors. Engineered stem cell treatments for orthopedic injuries can also be done faster than traditional techniques.
Applicable in gene therapy, the future of this therapy lies in repairing damaged bone using stem cells. This form of treatment is more effective than a patient undergoing physical therapy and potentially results in a faster recovery time. This method is also more cost-effective, as it eliminates the need for artificial bone replacements.
5. Pedicle screw
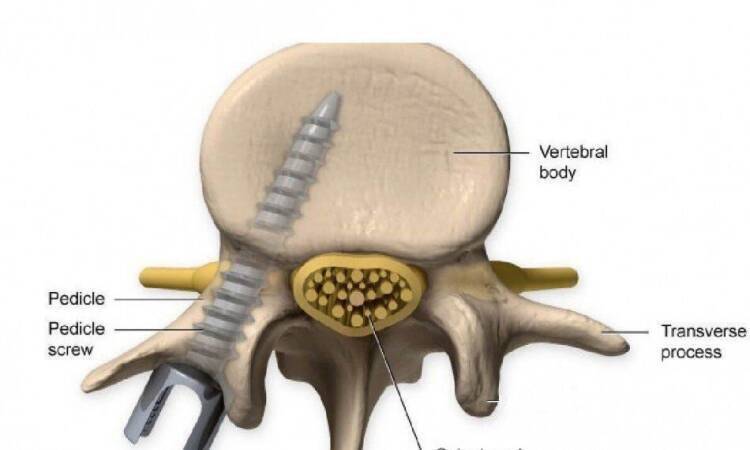
Vertebral body injuries are often treated by spinal fusion, which requires two adjacent vertebrae to be fractured and then stabilized with a rod, plate, and screws. A better alternative is pedicle screw fixation, where the screw is inserted into the anterior aspect of the pedicle and has a better purchase to hold it there. This makes the screw more stable thus improving fixation infusions.
The main problem with pedicle screw fixation is that the fixation screws will be extracted after fusion. Thus, the screws have to be regularly removed and reinserted which can cause a significant loss of tissue. Several studies have shown that re-insertion of a pedicle screw is not effective, especially in cases where there has been damage to the pedicle, vertebrae, or surrounding soft tissues. However over the years, with the best use of the pedicle screw and the minimal losses of tissue, this method has become a popular procedure in the fusion field.
6. Magnetic resonance imaging (MRI)

Superconducting magnets found in MRI machines, which generate large magnetic fields, allow for improved detection of soft-tissue abnormalities. These abnormalities can be detected and treated soon after their development, rather than relying on patients seeking care for pain over time. The use of MRI has resulted in many diagnostic procedures that have been extremely beneficial for orthopedic surgeons and patients alike.
The radiofrequency coils used in MRI machines, for instance, permit the imaging of bones through bone. In the past, for example, surgeons had trouble finding clear images of fractures or dislocations in patients. The use of radiofrequency helped to alleviate this difficulty by imaging fractures or dislocations as well as bone infections and swelling.
Orthopedic physicians have also been able to determine a patient’s injury origin more accurately through the use of MRI technology. Growing evidence supports the use of MRI tracking to determine the source of patient pain. This helps physicians choose the appropriate treatment and reduces the chance of misdiagnosis.
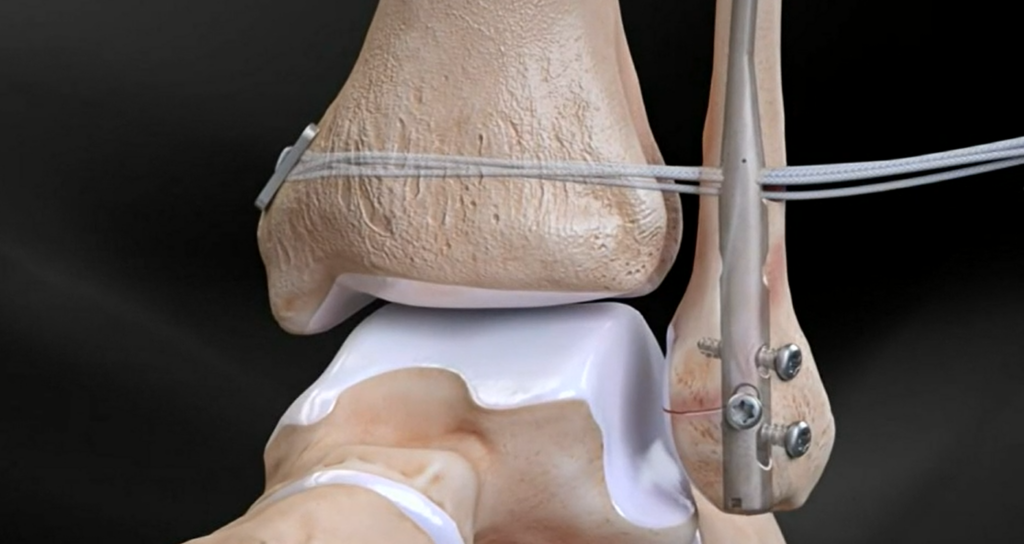
7. External fixator

Using a metal frame to fix broken bones has been around for a while and they were first used in the Civil War. What is important to note is that during this time or before this, casts would be used to stabilize the broken bone. Casts are effective, but they encase the entire injured limb, which can lead to muscle atrophy and soft-tissue edema. The external fixator allows for a more targeted approach as it does not restrict the movement of any part of the injured limb.
With time, the external fixator has also become smaller and more functional as it is now possible to drill holes in the bone and lay wires across these holes which can be used for fixation. This reduces the overall chance of infection as well. As a mainstay in the treatment of muscle-powered injuries, the external fixator has also been used to reduce muscle atrophy. The technique has been widely accepted, especially in the military, where it has been widely used during combat.
As medicine continues to advance, awareness of orthopedic conditions has gone up exponentially. This has led to greater understanding and sensitivity concerning pain management. Because of this increased awareness and the availability of new diagnostic procedures and treatment protocols, physicians can recommend treatments that are more effective and better targeted at addressing orthopedic issues. The field of orthopedic medicine has grown over the years, and it continues to progress in terms of both technology and research. Advances in orthopedics will invariably translate into improved quality of life for patients.




